Should caution be exercised in the rollout of covid-19 vaccines to NZ children from 5 years old? History indicates rushed decisions lead to regret.
Gerhard Sundborn,1* Simon Thornley,2 Rupert Scott,3 René de Monchy,4 Matt Shelton,5 Byram Bridle6
Lecturer in Pacific Health, University of Auckland, Department of Pacific Health, New Zealand 1
Epidemiologist/Public Health Physician, University of Auckland, Section of Epidemiology and Biostatistics, New Zealand 2
General Practitioner, Whangarei, New Zealand 3
General Practitioner and Psychiatrist, Tauranga, New Zealand 4
General Practitioner, Wellington, New Zealand 5
Professor of Viral Immunology, University of Guelph, Canada6
Corresponding author * email: g.sundborn@auckland.ac.nz
The New Zealand Ministry of Health have indicated that they are now actively considering the Pfizer covid-19 vaccine for New Zealand Children age from 5 to 11 years old.1 This follows its approval for use in New Zealand children aged 12 to 15 years on Monday 21st June, by ‘Medsafe’, New Zealand’s drug regulator.2 Other countries including USA, Canada, China and the European Commission who have also approved the vaccine for children aged 12 to 15 years old. China has authorised vaccination for children from three years of age. However, the World Health Organization (WHO) advise that children and adolescents have milder disease than adults and therefore more evidence is needed on different covid-19 vaccines for this age group, which has prevented them from making general recommendations for their use.3 In the UK the Joint Committee on Vaccination and Immunisation (JVCI) concluded that the health benefits gained by vaccination of 12 – 15 year old children are only marginally greater than the potential and known harms. And that this margin of benefit was too small to support universal vaccination of healthy 12 to 15 year old children.4 Since covid-19 itself poses little risk of fatality to children, and the exposure to a vaccine entails risks which are now poorly understood, we examine them in more detail here. Recently, an Auckland Professor of Epidemiology, regarding covid-19 vaccination stated:
“The Government has introduced (vaccine) mandates in health – total no-brainer. They’ve also introduced one in education for all the staff – total no-brainer. They need to introduce the same mandate for 12-and-over children”.5
To date, a decision to rollout the vaccine to children aged 5 – 11 years has not been made. We question the idea that vaccine mandates are a “no-brainer” particularly for children. Specifically, we believe that for children, emerging data indicates that such a policy will lead to more harm than good. We urge a precautionary approach be taken and that any plans for the vaccination of children be delayed for three important reasons.
Long-term safety and efficacy of the covid-19 vaccine is unknown: The first and most crucial point is that the long-term safety and efficacy data from the trial will not be available until 2023. Although short-term safety and efficacy data looks promising, this has only been tested in a small cohort of children, with 1,131 children receiving the vaccine at the time of writing.6 This means that detected adverse effects would only be those which are relatively common, and side effects, such as excess clotting that have led to the withdrawal of the AstraZeneca vaccine, for example, from many countries would not have been detected.7 This vaccine is one of the fastest to ever be developed and rolled out, taking less than one calendar year. Before this, the fastest approval was four years. Most take an average of ten to fifteen years from development to approval for clinical use.8
When we reflect on the 2009 swine flu pandemic a similar scenario occurred where the hastened development and approval of a vaccine took an astonishing 5-6 months once the new virus was identified.9 The vaccine was then administered widely, until 2011-12 when long term safety and efficacy data were available – from which studies indicated that the vaccine caused unacceptable rates of narcolepsy.10 This resulted in over a billion-dollars’ worth of these vaccines being destroyed.11-13
Another more distressing example occurred in the 1976 swine flu outbreak at the US Fort Dix military base. The infection caused one death and 230 soldiers to become ill. This led to a hastily developed vaccine that was rolled out to approximately 22% of the US population. The resulting vaccine caused over 500 cases of paralysis and 25 deaths. The vaccine was far worse than the virus itself and observers thought that the government response was too fast, with important safety considerations overlooked.14
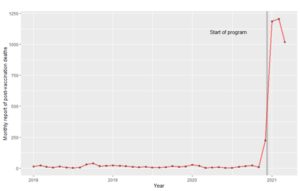
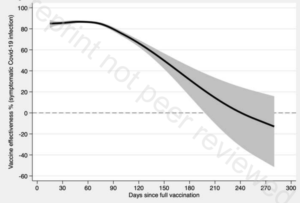
In the US there has been a dramatic increase observed in US government vaccine injury reports as evidence of vaccine harm. The 100-fold increase in post-vaccine deaths reported in temporal association to the rollout of the Covid-19 vaccines in late 2020 is perhaps best shown in the plot below.
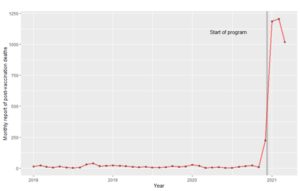
Figure 1. Time series of monthly reports of post-vaccine deaths to the US VAERS monitoring system.
Such a rapid increase in reports should be cause for concern, particularly when the development and clinical testing of the vaccines has been so truncated, and adverse effects from wide scale vaccination are unknown.15 Conventional epidemiological knowledge confirms that medical adverse event databases generally under-report safety signals. In a United States study that compared augmented electronic monitoring of health records in the thirty days post-vaccination, with prompting of clinicians to report likely vaccine-related events to usual practice, the augmented system resulted in a 30-fold increase in vaccine-related incident reporting, compared to historical periods. 16 When considering whether the spike in adverse event reporting is related to increased rates of vaccination or harm due to the vaccine, statistical tests carried out by Rose et. al. indicate clearly that the deaths are clustered around the time immediately after the event, in a manner which is incompatible with what would be expected if such deaths were occurring due to background mortality risks (P < 0.001).17
Efficacy of the Pfizer covid-19 vaccine is reported to be 52% after the initial dose and 95% after the second dose which has been taken from interim data.18 However, these claims have been questioned by researchers in Israel who have seen a far lower than expected decline in cases following vaccination of over 75% of their elderly population. Rather than a 52% decline in cases they have seen a significantly lower reduction in cases by 33%.19 Further, the protection against new variants of the virus remains unknown. A study recently published in the Lancet has found being fully vaccinated does not reduce any transmissibility once infected with the virus, compared to unvaccinated infected people.20
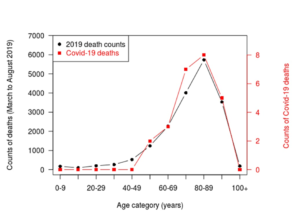
Very recently published evidence from overseas, where the vaccine rollout has occurred earlier than in New Zealand shows that vaccines are not resulting in enduring and lasting protection from the virus. A preprint Swedish cohort study (1.6 million people) which compares the risk of Covid-19 infection in vaccinated and unvaccinated people throughout the Covid-19 vaccination roll-out in the country from the 4th of January to the 4th of October 2021.21 Analysis of those who had taken the Pfizer vaccine showed that the effectiveness at preventing symptomatic infection waned from initial high levels to 47% in the period 121-180 days after the vaccine to no convincing effect beyond day 211 post-vaccination (23% reduction; 95% confidence interval, -2 to 41, P = 0·07), compared to unvaccinated people. This modelled decline in vaccine effectiveness is illustrated in the figure below. Such an effect was observed for all Covid-19 vaccinations used in the country, and observed for more severe health outcomes such as prevention of Covid-19 hospitalisation and death.
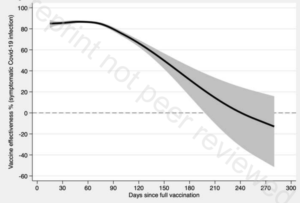
Figure 2. Estimated adjusted effect of vaccine to prevent Covid-19 infection after vaccination in Sweden.21 Solid line represents point estimate and shading represents 95% confidence interval. Overall, no beneficial effect is observed after 240 days (8 months) since vaccination.
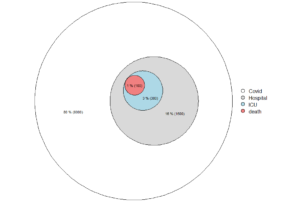
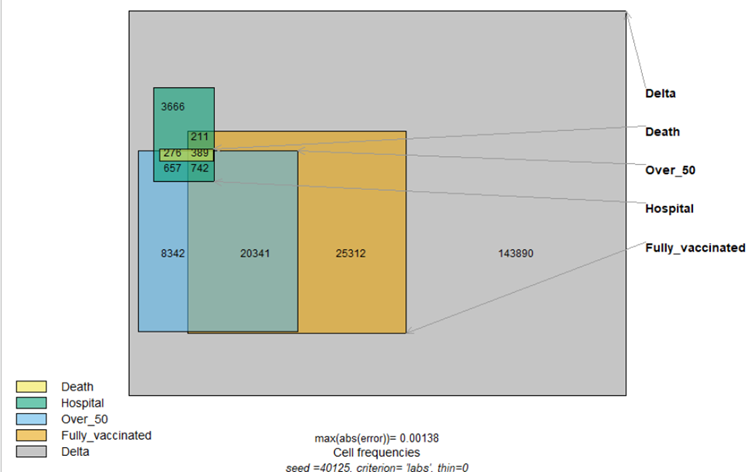
The risk covid presents to children is negligible: The second reason against vaccinating children is the very small risk that the virus poses to this group.22 There is a 1,000-fold difference in mortality risk between comparing children with frail elderly people after testing positive for covid-19. It is extraordinarily rare for a child to suffer any significant illness from covid-19 and orders of magnitude more rare for them to die from this virus.23 A prominent US epidemiologist likened the risk of a person less than 65 years old dying from covid-19 as remarkably uncommon and about the same as dying during a car journey from between 21 – 162 km each day.24 This comparison shows that there is little personal risk posed by covid-19 to children and thus no reason to expose them to an experimental vaccine. Other arguments for vaccinating children are related to the threat of ‘asymptomatic transmission’. Up-to-date evidence, however, shows little evidence of this phenomenon in Wuhan, after 10 million people were screened by PCR for infection, whether or not they had symptoms.25
Vaccine-associated risks that need further investigation: To date 18 countries including Canada, Sweden, Latvia, Germany, Italy, France, Spain, Denmark, Norway, and The Netherlands, have halted the roll-out of the AstraZeneca covid-19 vaccine due to concerns that it has caused blood clots in some recipients.6 There are similar concerns that the Pfizer vaccine may also cause clots. In Norway, 23 deaths of frail elderly people occurred shortly after receiving the Pfizer vaccine – with an investigation concluding that the vaccine was responsible for at least 10 of these deaths.26 In Australia two middle-aged women also died after receiving the AstraZeneca vaccine, caused by rare blood clots in the brain.27
Another risk from the vaccine for young people that have received the Pfizer or Moderna vaccine is myocarditis or pericarditis. In the US, more than 1,200 such cases have been identified in people younger than thirty years according to the Centres for Disease Control. A study in the United States showed that the risk of myocarditis after vaccination was 3.7 to 6.1 times higher than the risk of hospitalisation due to covid-19, even under conditions of moderate and high covid-19 incidence.28 A more recent study shows a 13.6-fold (1,260%) increase in new cases of myocarditis after the second vaccine in 16 to 19 year old males, compared to background rates of the disease in the same demographic group between 2017 and 2019.29 Other authors have questioned the use of vaccines in anyone less than the age of 65 years, since deaths attributable to the vaccine are likely to outnumber those saved by a factor of five.30 For younger children, this calculation is even less favourable. These events have generally occurred within a week following receiving the second dose of the vaccine.31
Under-reporting into vaccine safety databases is common. In a United States study that compared augmented electronic monitoring of health records in the thirty days post-vaccination, with prompting of clinicians to report likely vaccine-related events to usual practice, the augmented system resulted in a 30-fold increase in vaccine-related incident reporting,32 compared to historical periods. This means that analyses based on such reporting systems are likely to be gross underestimates of the true burden of adverse events.
Other academics overseas have expressed concerns at the high rate of post-vaccine adverse effects reported in vaccine safety databases. In the UK ‘Yellow card’ system, for example, between 4 Jan and 26 May 2021, a total of 1,253 deaths and 888,196 adverse reactions post covid-19 vaccine were recorded, with 63 million people receiving at least one dose, and 24 million having had two doses. This is roughly a 1/50,000 risk of death and 1/70 risk of adverse reaction after vaccination, assuming these reports are all caused by the vaccine. The author of the document, Dr Tess Lawrie, stated that based on these figures there was: “more than enough evidence … to declare the COVID-19 vaccines unsafe for use in humans”.33
Table 1. Adverse Events for Covid-19 Pfizer vaccine verses influenza vaccine in NZ
| |
Covid-19
Vaccine
2021 |
Influenza Vaccine 2019 |
| Adverse Events Following Vaccination
(AEFI) |
27,651 |
229 |
| AEFI Rate |
477/100,000 |
15.2/100,000 |
| Adverse Events of Special Interest |
982 |
– |
| Death following vaccination |
91 |
– |
| Doses administered |
5,792,114 |
1,505,268 |
Reviewing the latest Covid-19 vaccine safety report from Medsafe (New Zealand Medicines and Medical Devices Safety Authority) published on 9 October 202134 – a total of 27,651 Adverse Events following Vaccination (AEFI) have occurred. With 982 of these being Adverse Events of Special Interest (AESI) which are paid greater attention due to their seriousness. Most concerning is the number of deaths that have occurred following vaccination which now totals 91. When comparing the number of adverse events from the covid-19 vaccine to those reported to Medsafe for the influenza vaccine in 2019, 35 we calculate that the Covid-19 vaccine adverse events rate is more than 31-fold greater. Further the influenza vaccine has no reports of Adverse Events of Special Interest, nor death following vaccination. From these data the covid-19 vaccine exposes those who receive it to far higher rate of adverse health consequences than that for influenza.
Summary: The Pfizer covid-19 vaccine remains experimental and is only provisionally approved for use in New Zealand. Long-term safety and efficacy data will not be known until 2023, and children are largely unaffected by the virus. Like the swine flu vaccine, a true understanding of the long-term side-effects of the vaccine remain unknown until these trials are complete. There are several serious side effects caused by current covid-19 vaccines whose risks are not fully understood. Basic safety biodistribution studies are missing,36 with data from rodent models showing high uptake of nanoparticle delivery substrate in the ovaries of these animals.37 Basic safety studies, that are a routine part of vaccine development were not carried out for this vaccine.
When considering whether to vaccinate children against covid-19, one must weigh the therapeutic benefits against the risks. With such little to gain, all children can possibly experience are the risks of the product, such as myocarditis. True estimates of risks from the vaccine are now not fully understood, although there are already several identified now including blood clots, myocarditis, and death. 38, 39, 34
On balance, we believe that the known and unknown risks from the vaccine outweigh any benefits for children. Historical examples should lead us to pause and make a sober assessment of the risks, given the lack of benefit to children. We believe that it is best to wait at least two years for the long-term safety and efficacy results to enable a more informed decision to be made about whether to vaccinate children against SARS-CoV-2. Whatever else can be said about the decision to vaccinate children, it cannot and must not be considered a “no brainer”. No sober analysis would come to that conclusion.
This research did not receive any specific funding.
The authors declare no conflicts of interest.
References
1. 1 News. Children could be next in line for covid-19 vaccine. Monday 13 September 2021. Accessed 4 October 2021. https://www.tvnz.co.nz/one-news/new-zealand/children-could-next-in-line-covid-19-vaccine
2. Neilson M and Cheng D. Covid 19 coronavirus: Medsafe approves Pfizer vaccine for New Zealand 12-15 year olds. [Internet] New Zealand Herald. 21 June 2021. [cited 9 July 2021] Available from: https://www.nzherald.co.nz/nz/covid-19-coronavirus-medsafe-approves-pfizer-vaccine-for-new-zealand-12-15-year-olds/3D2OPZZLOPOOMXY6LJT43Z4F2A/
3. WHO. COVID-19 Advice for the Public: Getting Vaccinated. [Internet] WHO. 22 June 2021. [cited 9 July 2021] Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines/advice
4. Public Health England. Joint Committee on Vaccination and Immunisation. JVCI issues updated advice on COVID-19 vaccination of children aged 12 to 15. Published 3 September 2021. Accessed 4 October 2021. https://www.gov.uk/government/news/jcvi-issues-updated-advice-on-covid-19-vaccination-of-children-aged-12-to-15
5. Wilkins, Alice. Coronavirus: Expert calls for mandatory student vaccinations as senior high schoolers in level 3 return for in-person learning. Newshub. 25 October 2021. https://www.newshub.co.nz/home/new-zealand/2021/10/coronavirus-expert-calls-for-mandatory-student-vaccinations-as-senior-high-schoolers-in-level-3-return-for-in-person-learning.html
6. Pfizer. Pfizer-BioNTech Announce Positive Topline Result of Pivotal COVID-19 Vaccine Study in Adolescents. [Internet] Pfizer. 31 March 2021. [cited 9 July 2021] Available from: https://www.pfizer.com/news/press-release/press-release-detail/pfizer-biontech-announce-positive-topline-results-pivotal
7. Dean G, Schuster-Bruce C. Sweden joins Germany, France and 15 other countries in suspending AstraZeneca’s vaccine over possible side effects. [Internet] Business Insider Australia. 16 March 2021. [cited 9 July 2021] Available from: https://www.businessinsider.com.au/astrazeneca-covid-vaccine-countries-suspend-denmark-thailand-batch-blood-clots-2021-3?r=US&IR=T
8. The History of Vaccines. Vaccine Development, Testing, and Regulation. [Internet] The History of Vaccines. 17 January 2018. [cited 9 July 2021] Available from: https://www.historyofvaccines.org/content/articles/vaccine-development-testing-and-regulation
9. WHO. Pandemic influenza vaccine manufacturing process and timeline. [Internet] WHO. 6 August 2009. [cited 9 July 2021] Available from: https://www.who.int/news/item/06-08-2009-pandemic-influenza-vaccine-manufacturing-process-and-timeline
10. Stranden AL. Norwegian study links flu vaccine to narcolepsy risk [Internet]; Science Norway, 28 March 2017; [cited 2020 Dec 17]. Available from: https://sciencenorway.no/forskningno-norway-vaccine/norwegian-study-links-flu-vaccine-to-narcolepsy-risk/1444067
11. Conner R. Germany to destroy expensive, unwanted swine flu vaccine [Internet]; Deutsche Welle, 17 August 2011; [cited 2020 Dec 17]. Available from: https://www.dw.com/en/germany-to-destroy-expensive-unwanted-swine-flu-vaccine/a-15324186
12. O’Callaghan T. Some 40 million doses of H1N1 vaccine to be destroyed [Internet]; Time, 1 July 2010; [cited 2020 Dec 17]. Available from: https://healthland.time.com/2010/07/01/some-40-million-doses-of-h1n1-vaccine-to-be-destroyed/
13. Independent. Netherlands destroying 17 million swine flu vaccine doses [Internet]; 18 September 2011; [cited 2020 Dec 17]. Available from: https://www.independent.co.uk/life-style/health-and-families/netherlands-destroying-17-million-swine-flu-vaccine-doses-2038287.html
14. Khamsi, Roxanne. How we will know when coronavirus vaccine is ready. [Internet] National Geographic. 1 July 2020. [cited 2021 July 7] Available from: https://www.nationalgeographic.com/science/2020/06/how-we-will-know-when-coronavirus-vaccine-is-ready-cvd/
15. Seneff et al “Worse Than the Disease? Reviewing Some Possible Unintended Consequences of the mRNA Vaccines Against COVID-19” Vol. 2 No. 1 (2021): Epidemic NCDs https://www.ijvtpr.com/index.php/IJVTPR/article/view/23
16. Meghan A. Baker, David C. Kaelber, David S. Bar-Shain, Pedro L. Moro, Bob Zambarano, Megan Mazza, Crystal Garcia, Adam Henry, Richard Platt, Michael Klompas, Advanced Clinical Decision Support for Vaccine Adverse Event Detection and Reporting, Clinical Infectious Diseases, Volume 61, Issue 6, 15 September 2015, Pages 864–870, https://doi.org/10.1093/cid/civ430
17. Rose J. A Report on Myocarditis Adverse Events in the U.S. Vaccine Adverse Events Reporting System (VAERS) of the COVID-19 Messenger Ribonucleic Acid (mRNA) Biologicals. Science, Public Health Policy, and The Law. Volume 2:59-80. May, 2021.
18. Mahase E. Covid-19: Pfizer vaccine efficacy was 52% after first dose and 95% after second dose, paper shows BMJ 2020; 371: m4826 doi:10.1136/bmj.m4826
19. Mahase E. Covid-19: Reports from Israel suggest one dose of Pfizer vaccine could be less effective than expected. BMJ. 2021 Jan 22;372:n217. doi: 10.1136/bmj.n217. PMID: 33483332
20. Singanayagam A, Hakki S, Dunning J, Madon KJ, Crone MA, Koycheva A, et al. Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study. Lancet Infect Dis 2021 Published Online October 28, 2021 https://doi.org/10.1016/ S1473-3099(21)00648-4
21. Nordström, Peter and Ballin, Marcel and Nordström, Anna, Effectiveness of Covid-19 Vaccination Against Risk of Symptomatic Infection, Hospitalization, and Death Up to 9 Months: A Swedish Total-Population Cohort Study. Available at SSRN: https://ssrn.com/abstract=3949410 or http://dx.doi.org/10.2139/ssrn.3949410
22. Bhopal SS, Bagaria J, Olabi B, Bhopal R. Children and young people remain at low risk of COVID-19 mortality. Lancet Child Adolesc Health. 2021 May;5(5):e12-e13. doi: 10.1016/S2352-4642(21)00066-3. Epub 2021 Mar 11. Erratum in: Lancet Child Adolesc Health. 2021 Mar 24;: PMID: 33713603; PMCID: PMC7946566.
23. Battacharya J. Opinion: Jay Bhattacharya: A compassionate covid strategy. [Internet] NWA Online. 15 November 2020. [cited 9 July 2021] Available from: https://www.nwaonline.com/news/2020/nov/15/compassionate-covid-strategy/
24. Ioannidis JPA, Axfors C, Contopoulos-Ioannidis DG. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ Res. 2020 Sep;188:109890. doi: 10.1016/j.envres.2020.109890. Epub 2020 Jul 1. PMID: 32846654; PMCID: PMC7327471.
25. Cao, S., Gan, Y., Wang, C. et al. Post-lockdown SARS-CoV-2 nucleic acid screening in nearly ten million residents of Wuhan, China. Nat Commun 11, 5917 (2020). https://doi.org/10.1038/s41467-020-19802-w
26. Torjesen I. Covid-19: Pfiver-BioNTech vaccine is “likely” responsible for deaths of some elderly patients, Norwegian review finds BMJ 2021; 373 :n1372 doi10.1136/bmj.n1372
27. Davey M. ‘Extremely rare’: Australia records second death ‘likely linked’ to AstraZeneca vaccine blood clots. [Internet] The Guardian. 10 June 2021. [cited 9 July 2021] Available from: https://www.theguardian.com/australia-news/2021/jun/10/extremely-rare-australia-records-second-death-likely-linked-to-astrazeneca-vaccine-blood-clots
28. Hoeg T, Krug A, Stevenson J, Mandrola J. SARS-CoV-2 mRNA Vaccination-Associated Myocarditis in Children Ages 12-17: A Stratified National Database Analysis. medRxiv preprint posted 8 September 2021. https://www.medrxiv.org/content/10.1101/2021.08.30.21262866v1.full.pdf
29. Mevorach D, Anis E, Cedar N, Bromberg M, Haas EJ, Nadir E, Olsha-Castell S, Arad D, Hasin T, Levi N, Asleh R, Amir O, Meir K, Cohen D, Dichtiar R, Novick D, Hershkovitz Y, Dagan R, Leitersdorf I, Ben-Ami R, Miskin I, Saliba W, Muhsen K, Levi Y, Green MS, Keinan-Boker L, Alroy-Preis S. Myocarditis after BNT162b2 mRNA Vaccine against Covid-19 in Israel. N Engl J Med. 2021 Oct 6:NEJMoa2109730. doi: 10.1056/NEJMoa2109730. Epub ahead of print. PMID: 34614328; PMCID: PMC8531987.
30. Kostoff RN, Calina D, Kanduc D, Briggs MB, Vlachoyiannopoulos P, Svistunov AA, Tsatsakis A. Why are we vaccinating children against COVID-19? Toxicol Rep. 2021;8:1665-1684. doi: 10.1016/j.toxrep.2021.08.010. Epub 2021 Sep 14. Erratum in: Toxicol Rep. 2021 Oct 7;: PMID: 34540594; PMCID: PMC8437699. https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8437699/pdf/main.pdf
31. Lovelace B. CDC safety group says there’s a likely link between rare heart inflammation in young people after Covid shot. [Internet] CNBC. 23 June 2021. [cited 9 July 2021] Available from: https://www.cnbc.com/2021/06/23/cdc-reports-more-than-1200-cases-of-rare-heart-inflammation-after-covid-vaccine-shots.html
32. Meghan A. Baker, David C. Kaelber, David S. Bar-Shain, Pedro L. Moro, Bob Zambarano, Megan Mazza, Crystal Garcia, Adam Henry, Richard Platt, Michael Klompas, Advanced Clinical Decision Support for Vaccine Adverse Event Detection and Reporting, Clinical Infectious Diseases, Volume 61, Issue 6, 15 September 2015, Pages 864–870, https://doi.org/10.1093/cid/civ430
33. Trialsite staff. Look into UK Yellow Card System Reveals Large Numbers of Adverse Events and Deaths Associated with COVID-19 Vaccine. [Internet] Trial Site News. 10 June 2021. [cited 9 July 2021] Available from:
34. https://trialsitenews.com/wp-content/uploads/2021/06/Yellow-Card-Letter.pdf
35. Medsafe. Adverse events following immunization with COVID-19 vaccines: Safety Report #32 – 9 October 2021. Published 9 October 2021. Accessed 31 October, 2020. https://www.medsafe.govt.nz/COVID-19/safety-report-32.asp
36. Medsafe. Spontaneous reports: Seasonal influenza vaccination 2020. Revised1 April 2021. Accessed 4 October, 2020. https://www.medsafe.govt.nz/safety/reports-and-promotion/Spontaneous-Reports-Influenza-Vaccination-2020.asp#More
37. Doshi P. Covid-19 vaccines: In the rush for regulatory approval, do we need more data? BMJ 2021; 373 :n1244 doi: 10. 1136/bmj.n1244 Available from: https://www.bmj.com/content/373/bmj.n1244
38. Joan-Ramon Laporte, Ermengol Coma, Francesc Fina, Luís García-Eroles, Xavier Vidal, Manuel Medina. Vaccines against Covid-19, venous thromboembolism, and thrombocytopenia. A population-based retrospective cohort study. MedRxiv preprint; this version posted September 5, 2021. Date accessed: 4 October 2021. doi: https://doi.org/10.1101/2021.07.23.21261036
39. Marshall M, Ferguson ID, Lewis P, et al. Symptomatic acute myocarditis in seven adolescents following Pfizer-BioNTech COVID- 19 vaccination. Pediatrics. 2021; doi: 10.1542/peds.2021-052478