Simon Thornley, Ananish Chaudhuri
1258 words.
António Egas Moniz was awarded the Nobel Prize in 1949 for frontal lobotomy, a supposed cure for mental illness. Ultimately, however, Moniz and the Nobel committee were wrong. The operation did irreparable harm to over fifty thousand patients and the results were far from the claimed ‘cure’.
Early in New Zealand’s Covid-19 story we were admonished with predictions of 80,000 covid-19 deaths by Professor Sean Hendy and his colleagues, even with stringent lockdowns in place. Recently, Professor John Gibson questioned the accuracy of these predictions as implausible because they would require our population to be almost 10-times larger, to square with the infection-fatality proportion reported by the WHO for countries like us. Yet Hendy doubled down on the predictions. Considering that New Zealand now has 26 official Covid-19 deaths, it seems at face value that Gibson is right. Hendy overshot the mark. By a lot.
What is remarkable now is the lack of insight into why these predictions were wrong. We have now learned so much more about Covid-19, we must update our ideas. The government’s own advice to its new Minister shows that Hendy’s exaggerated prediction will have enormous costs to New Zealand society. Crown debt is forecast to grow by 2.5 times to a level of NZ$200 billion in 2024, and the real value of output in 2020 is over five percent smaller than what had been forecast in 2019.
With so much at stake, it is essential that we take stock of what we have learned and why Hendy and his colleagues erred. After all, science is little more than the recalibration of our beliefs and predictions to match the stark reality of collected data. From what Hendy indicated in his response with revised predictions of 10,000 deaths he has learned little about the virus since the early forecasts. His response centred on explanations such as: vaccines arriving early, a modest change in the infection fatality rate (0.9% is the new value, compared to 1.0%), and the lack of capacity in intensive care.
What is most remarkable about these explanations is that none of them could possibly explain the discrepancy between Hendy’s original model and the observed deaths. Since the deaths are simply a proportion of the overall cases (infection fatality ratio), a 10% change can in no way explain the difference between models and reality, which differ by three orders of magnitude (3,076 times).
So, what have we learned about Covid-19 and why were Hendy’s models wrong? First, the models assumed the virus was totally new and that the entire New Zealand population was susceptible. Many studies now show that cross-reactivity and T cell responses to other coronaviruses protect us from Covid-19. Many of us will simply shake off the virus since our immune systems have already seen similar ones.
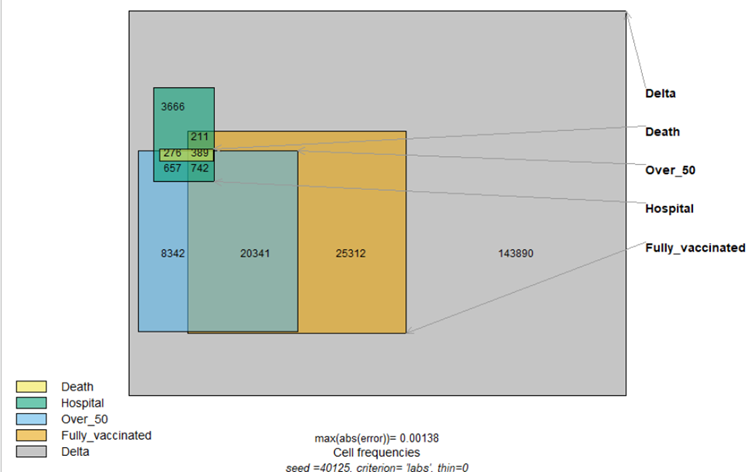
Hendy takes it as a given that Covid-19 is ten times more deadly than influenza, with no evidence cited. Calculating the ‘deadliness’ of a virus is a difficult issue, since it is dependent on accurately estimating cumulative numbers of infection – the denominator, as well as Covid-19 deaths – the numerator. Deaths are sensitive to definitions of what exactly constitutes a Covid-19 death, particularly in the frail elderly, who often have a range of other diseases.
To illustrate, Singapore has a strict definition of Covid-19 deaths, which requires a positive test and respiratory infection leading to death. The city state has registered only 30 deaths out of 60,019 cases (case fatality ratio: 0.05%). In contrast the UK, which has a comparatively loose definition, including all who died within a period of testing positive, has a case fatality ratio of 2.9%, 40 times higher than Singapore, from the same virus. The most comprehensive survey of infection fatality ratios, which account for positive serology, has yielded a corrected median of 0.23%, well under Hendy’s estimate. This figure does not account for T cell responses to the virus, and takes death recording at face value.
Evidence from wastewater in Barcelona and retrospective analysis of blood samples from a lung cancer screening study in Italy suggests that SARS-Cov-2 was circulating in Italy before its supposed discovery in Wuhan in December 2019. What do we learn from this? Since there was no excess death at that time, it cannot therefore be assumed that excess death that accompanied lockdowns is a direct consequence of the virus. Many of us have likely seen the virus and not known it, since it was circulating well before Wuhan, and health systems coped at that time.
It is remarkable also that Hendy’s doomsday predictions showed little appreciation of the age of deaths with Covid-19. Other authors predicted the magnitude of deaths in NZ from Covid-19 to those from World War 1, which averaged in the 20s of the soldiers who died. Spanish flu victims, similarly, had a median age of death in the twenties, but not those from Covid-19. The average age of deaths with Covid-19 are about the same as the life expectancy of that country. This means that the virus is certainly not as deadly as Hendy claims, since deaths from the virus will not lower the life expectancy of a population. Put another way, risk of death from the virus is no different to the background risks we face every day.
Hendy also fails to discuss the exaggeration in coding of Covid-19 deaths that has occurred during the pandemic. The fact that many deaths have been due to other illnesses and the usual process of recording death has been overturned. This panic induced exaggeration has also been a feature of many other historical epidemics of respiratory illnesses.
Another feature of the Covid-19 story is that much of the early high fatality was related to foregone opportunities for healthcare for other conditions. In the UK, emergency department visits halved during lockdown. To compound this, early mechanical ventilation in intensive care, which overloaded these units, inflated mortality from the virus. Statistical evidence now supports this policy as a cause of excess deaths in Covid-19 cases.
Hendy’s revised estimate that we must have saved at least 10,000 lives assumes lockdowns are effective. This is counter to the weight of statistical evidence on the subject. A between-country analysis showed no evidence that lockdowns save lives, either measured as a stringency index or from google mobility data.
We urgently need to return to the foundations of science which means a sober assessment of reality over failed forecasts. It seems Hendy is unlikely to champion such a cause, since his predictions have cost New Zealanders dearly. Wrong predictions are a routine part of science, but a stubborn adherence to them indicate a deviation from usual practise.
Our usual way of life, our ability to engage with the world, and much of our economy have been surrendered to erroneous predictions. Even with orders of magnitude differences from the reality of observed data, the author remains wedded to them.
The words of Nobel prize winner, Professor Richard Feynman are relevant:
“It doesn’t matter how beautiful your theory is, it doesn’t matter how smart you are. If it doesn’t agree with experiment, it’s wrong.”
Given what is at stake for New Zealand’s future, the last thing we now need is to cling to failed models. Rather, we must confront the frightening fact that much of what we initially thought we knew about Covid-19 was wrong. Dire predictions simply did not eventuate. The spectre of further lockdowns and strict border closures urgently need to be re-evaluated in this light. Feynman again:
“Reality must take precedence over public relations, for nature cannot be fooled.”

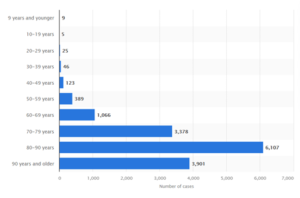 Figure. Deaths with covid-19 in Sweden, by age at November 3, 2021.
Figure. Deaths with covid-19 in Sweden, by age at November 3, 2021.