Drs Michael Jackson and Simon Thornley
A recent article in a New Zealand newspaper claims that Sweden’s approach to managing the Covid pandemic means that “56,000 more people may yet die”. We believe the article is misleading because:
- The author assumes an ‘infection fatality proportion’ (IFP) of 1% and states it’s the “current best estimate”. This estimate is derived from seroprevalence studies from just two countries (France and Spain – both with high per capita death rates). But, the Centre for Disease Control’s (CDC) recent best estimate is 0.26% (four times lower). A summary of studies (19 May) by Professor John Ioannidis that included studies from Asia, Europe, and North and South America derived an estimate of between 0.02% to 0.40%. This mirrors the IFR provided by the Centre for Evidence-Based Medicine at Oxford University. We believe the use of a high IFP is misleading as it produces an estimate that wasn’t based on current best estimates.
- The author does not include any commentary about the recent identification of cross-reactive T-cells. The paper’s findings (published May 14 and before the author’s article was published) indicate between 40-60% of a population may not even be susceptible to Covid-19 due to prior exposure to other coronaviruses that cause the common cold. This has important implications, as it lowers the number of people susceptible to infection. More recently (we acknowledge after the article was published), one of the world’s most influential neuroscientists and statisticians, Professor Karl Friston (University College London) said the figure could be as high as 80%. The inclusion of this information would have allowed for the re-calculation of an estimated fatality rate and provided the reader with further information about the uncertainty of the author’s predictions.
- The author assumes that 60% of a population needs to be have been infected or vaccinated to achieve herd immunity. But some are calculating it at 40% based on Sweden-specific data, not generic inputs. Also, the 60% figure is based on modelling, rather than measured seroprevalence. Given the previous data about T cell immunity and cross-reactivity of other antibodies, the true population immunity is likely to be much higher than seroprevalence surveys indicate. Again, this paints a more negative picture and doesn’t present the reader with a balanced view.
- The author states “After completing this article, a new study has reported that the proportion of people in Stockholm with antibodies to Covid-19 is only 7.3 per 100 people”. But an internet search will tell that the 7.3% figure “reflects the state of the epidemic earlier in April”. That’s a whole month before the article was written and when the total number of deaths in Sweden was around 1000. Sweden’s Public Health Agency estimates the figure would now be about 20% but this isn’t mentioned by the author.
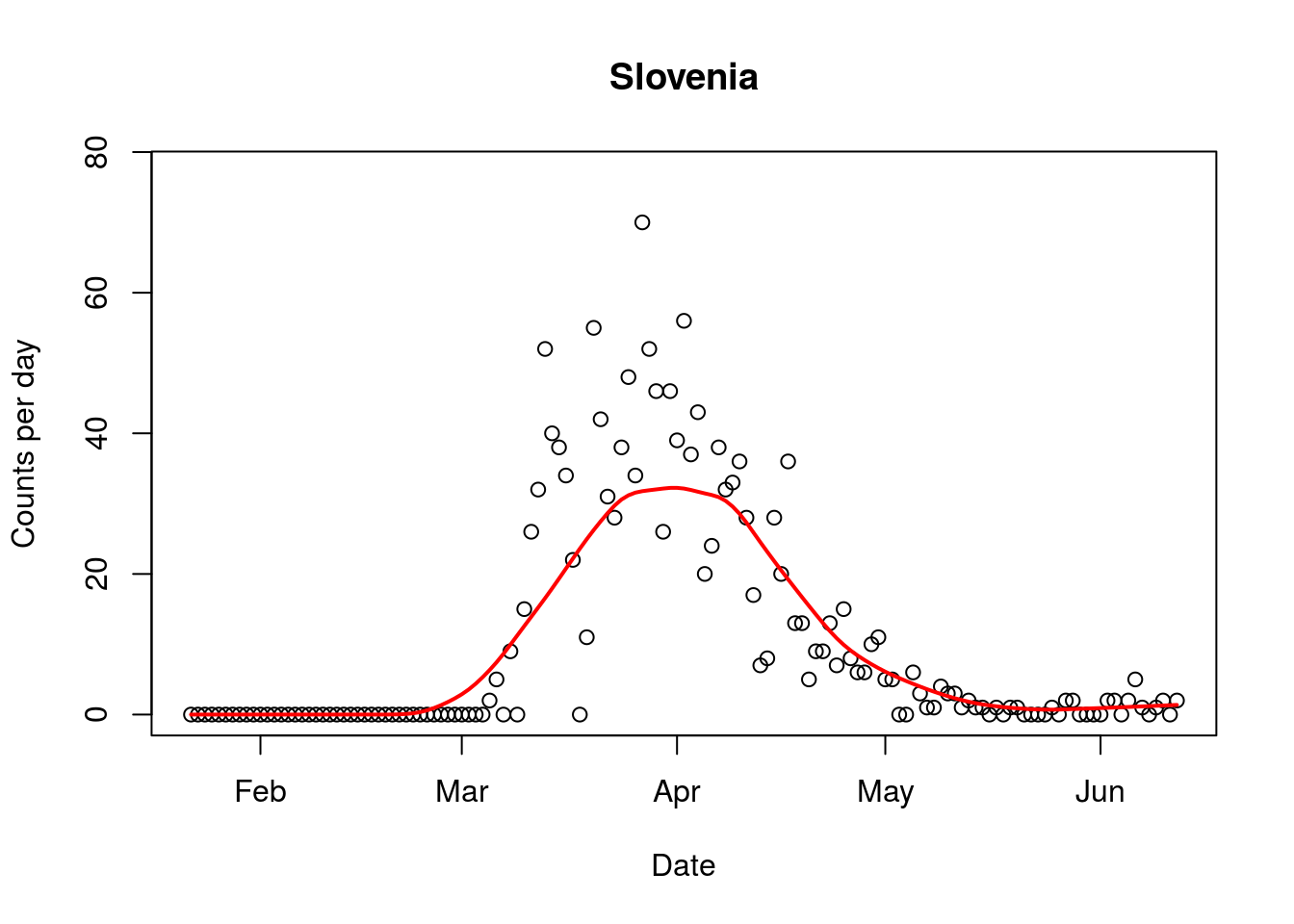
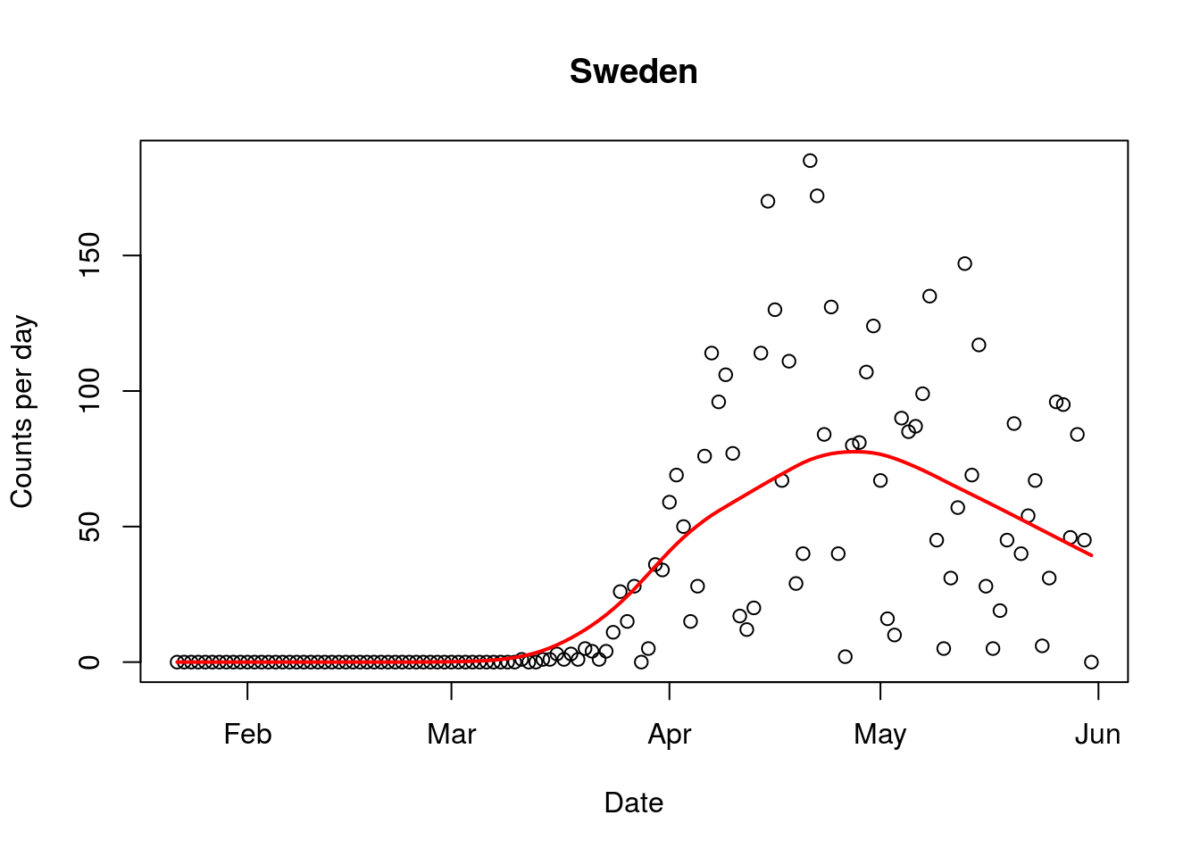
- The author does not attempt to consider how his prediction of 56,000 extra deaths matches actual recorded data and trends for Covid-19 in Sweden (figure). With 4,874 deaths currently, and a clear downward trend (also evident when the author published his article), the author’s prediction is unrealistic.
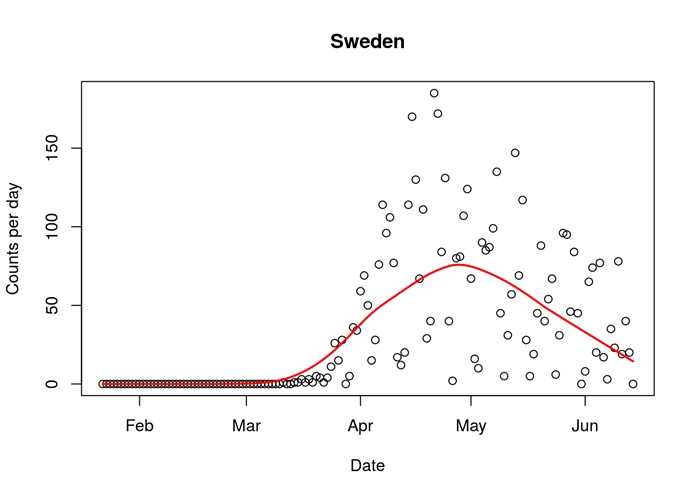 Figure. Covid-19 daily mortality in Sweden (16/6/2020). Line indicates trend.
Figure. Covid-19 daily mortality in Sweden (16/6/2020). Line indicates trend.
- The author claims that Sweden’s economy hasn’t fared any better than its neighbours, despite its more relaxed approach. Again, this is misleading. While this may be true for Denmark and Norway (note Norway now say they could have achieved the same results without a lockdown), Sweden’s projected downturn (1% GDP) is less than Germany (6.5%), the Netherlands (6.8%), the EU as a whole (7.4%), Belgium (8%), France (8.2%), Croatia, (9.1%), Spain (9.4%), Italy (9.5%), Greece (9.7%) and the UK (up to 14%). For comparison, the New Zealand government is predicting a downturn of around 10%. You may also be surprised to hear Sweden’s economy actually grew in the first quarter of 2020 compared to declines across Europe. The UK’s economy, for example, contracted by 2% over the same period.
We are not, here, looking to justify of Sweden’s approach. Only time will tell if Sweden took the right one. We are simply asking that commentators present their work in a balanced, evidence-based way – one that draws the reader’s attention to the complexity and uncertainty in their projections. Figures like “60,000 deaths” are headline-grabbing but are based on incomplete and overly simplistic modelling. They are not ‘reasonable best estimates” based and clearly contradict observed trends.