Simon Thornley
28 Feb 2021
New Zealand descends into another lockdown abyss just as I am now questioning the very foundations of the covid story.
Recently, I have pointed to evidence that covid was around in Europe before Wuhan. Since we were apparently living with covid in Europe without excess mortality or catastrophe, this seems at face value to suggest that we had lived with the virus and can do so again.
Another matter is that we have shifted how we define virus related factors, and this is causing us to believe SARS-CoV-2 is more serious than it is. Definitions are a cornerstone of epidemiology and the collection of scientific data. Death seems to be a clear-cut event in a person’s life but determining the cause of death is a surprisingly difficult process.
As Dennis De Nuto so beautifully illustrated in the Ocker flick, “The Castle”, definitions matter. Responding to the judge with “it’s the vibe, your honour” when alleging a constitutional law breach doesn’t quite cut it. While there is almost always uncertainty about causes of death and classification, this uncertainty has been stretched to breaking point in New Zealand’s covid-19 saga. The most recent death is illustrative.
We learned that an individual had been in quarantine. They were then transferred to North Shore Hospital for a serious non-covid illness and later tested positive for covid. The patient later died. A few days later, the death was considered another official NZ covid death. On the face of it, without further information, this does not indicate to me a death caused by infection with SARS-CoV-2. At no point in the article are we told that the individual had the disease that the virus is alleged to cause: a lung infection. When the reporter quizzed the Director General, Dr Ashley Bloomfield, for justification of the Ministry’s classification the response was revealing: ‘…we have been very inclusive in our approach of categorising deaths as covid-19-related…”. He went on to explain, “You might recall when we had a number of deaths last year sadly related to aged residential care. A number of those people had actually not been swabbed because of the nature of their conditions but they were categorised as probable cases because of their symptoms…”
We have learned two important things from these statements. In the first case, if you want to classify as a covid death you do not need evidence of a lung infection. In the second, when referring to the rest home deaths, you do not even need a positive PCR test. There was no further evidence related to autopsy or other clinical findings or investigations.
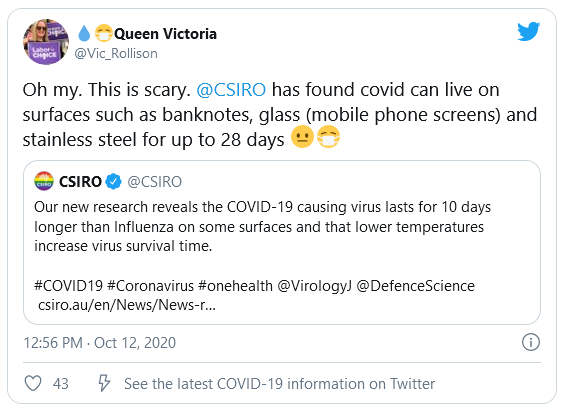
The next revelation came in how this decision making was justified. Bloomfield’s response was “Most countries are doing this, for example in the UK they categorise everyone who dies within 28 days of being hospitalised with covid-19 as … a COVID-19-related death.” Essentially, everyone else is doing it, so… why not?
It would be weird and totally unhelpful if this was the approach to any other disease. It’s even worse for Covid because we are now in Auckland’s fourth lockdown – justified based on saving lives from infection. It is now questionable that New Zealand’s covid-19 deaths would have lived longer without the infection. The absence of the virus clearly would be unlikely to have saved the latest death who was hospitalized with a “serious non-covid illness” and then tested positive. Not without further supporting information, which if present, has been withheld from the public domain.
Since it is also now stated that not all deaths tested positive, it is hard to be certain that the absence of the virus would have saved other ‘apparent’ covid deaths. Indeed, according to a June 2020 OIA request, five of the 21 deaths (at the time) reported tested either negative or had not been tested. This is important, since covid-19 is not a disease with specific signs and symptoms, it is unclear that the absence of the virus would have saved these negative or untested cases.
This now leaves the covid deaths who tested positive. We are simply not given enough clinical information to know whether these lives would be saved without the virus on board. What we do know is that 16/22 deaths at June 2020 occurred in rest home residents, and that 8/14 deaths until April occurred in residents of a specialized dementia unit. We also know that the age distribution of these deaths is no different from background. This is further evidence that the absence of SARS-CoV-2 would not have altered the survival of these people.
In Italy, the place that scared many of us into thinking the worst about covid-19, it has now been proved that covid deaths were systematically exaggerated. The same is likely in the United States.
The one country that bucks the trend and uses a strict definition of a covid-19 death is Singapore. It also happens to have 29 deaths from 59,925 cases at the time of writing, with a case-fatality ratio of 0.05%, less than for seasonal influenza. It may be definitions, rather than lockdown protocols, that means the virus has had little effect there. Rather ironically, lockdown enthusiasts in New Zealand have championed Singapore for its societal restrictions, but they have not championed its use of covid-related definitions.
It looks increasingly as if covid-19 is a kind of chimera, largely created by our own modern fears.
This is bizarre, as Auckland moves into its next lockdown, estimated to cost our economy half a billion dollars per week, and as the queues in food banks are expected to grow, with the lives of our poorest communities most affected.
We must scrutinise not only whether our strategy hell bent on elimination of this virus is worthwhile, but whether it’s even based on reality.